💊 Public Medications State Policy Briefing: Video and Notes
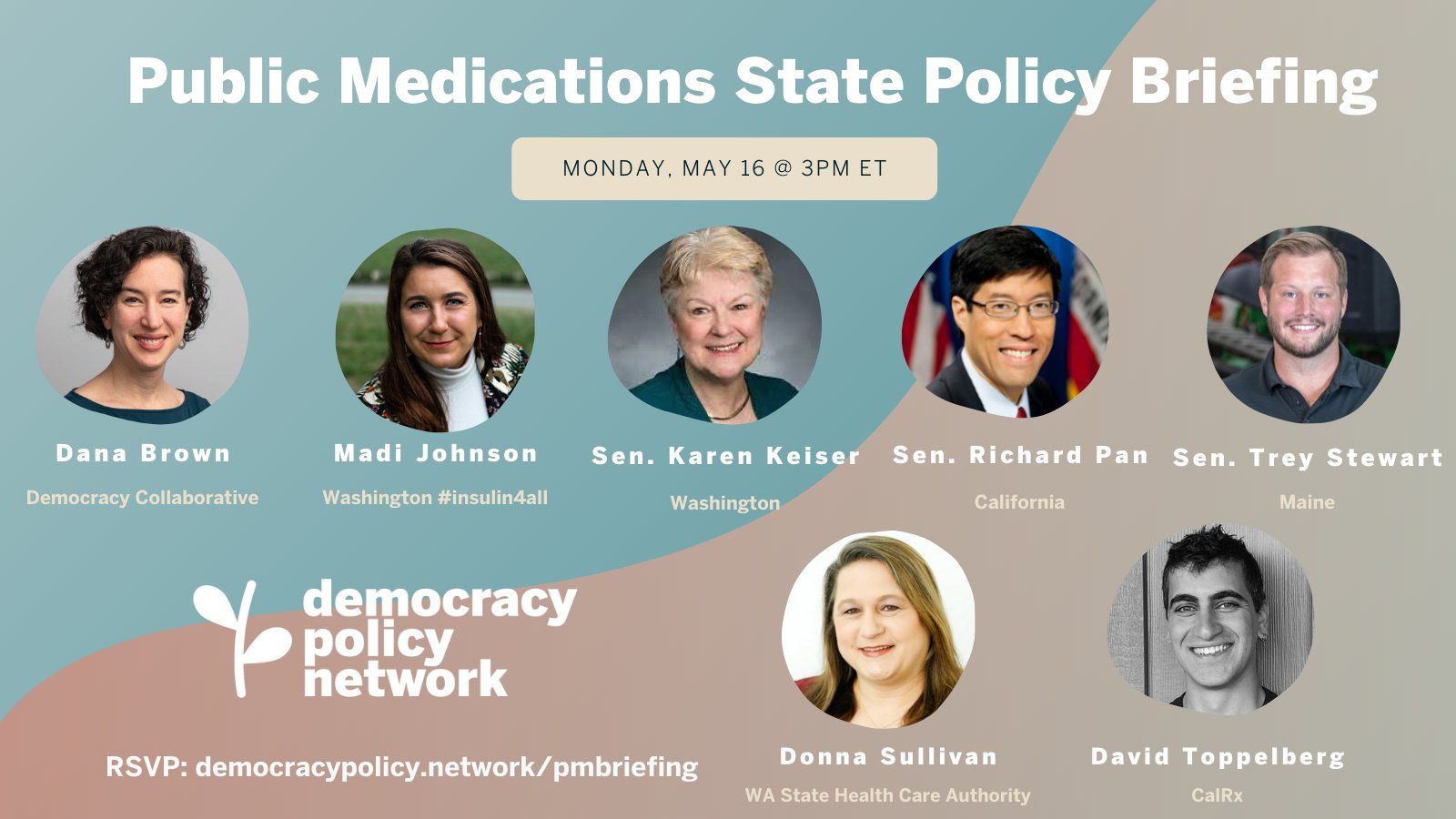
On May 16, DPN hosted a state policy briefing on Public Medications with experts, advocates, and legislators at the cutting edge of promoting publicly-owned pharmaceutical enterprises, created by states to develop, manufacture, and distribute medication in the public interest. Video and notes from the event are below.
Welcome — Pete Davis (Director, Democracy Policy Network)
Overview of the problem with monopolistic private medicine production — Madi Johnson (WA Chapter Leader, T1International)
- Some 1.6 million Americans are living with type one (T1) diabetes.
- One in four people living with T1 ration their insulin. They take less than they need to be happy and healthy because they cannot afford their insulin.
- Most vulnerable are under- or uninsured.
- Insulin prices have increased 6x in 20 years.
- Insulin is the bare minimum: Without it, in ~3 days you would not be alive.
- Insulin price has wildly outpaced normal inflation.
- Only three companies control 90%+ of global insulin production. There is no true generic insulin on the market. These companies will change the formula ever so slightly and re-patent it. This creates a 37 year patent in some cases.
Overview of the public medications model - Dana Brown (Director of Health and Economy, Democracy Collaborative)
- Public enterprises are not incentivized to profit-maximization and sector concentration—they can put focus on equity.
- A price cap does not center equitable access as well as public enterprises—it still hurts uninsured patients and continues to reward for-profit corporations with price control.
- In Brazil, public pharmaceutical initiatives supply medications to low-income populations with 100+ medications. Massachusetts produces some vaccines and Michigan used to. Many ways forward, including partnerships (with other public entities and with private entities) to create meds and distribute them across the country.
- The positive externalities of having populations with regular, affordable access to medications like insulin are huge: Saves health care costs on disease and treatment; helps people stay healthy and participate in workforce, communities.
California's SB852 and SB838 - Senator Richard Pan (CA)
- Senate committee on health had been exploring public medications for a while and Gov. Newsom proposed the same in his 2020 budget. This authorized California to manufacture generic medications, including insulin.
- Public meds will send signals in the market: if a hedge fund captured a drug, there might be another player entering.
- As a physician, Dr. Pan was aware of limitations in drug supply. Seeing the same thing with baby formula, now. Saw this with drugs for cancer treatments too.
- Manufacturing medications is not a simple task: highly regulated and takes sophistication and capital resources. California has authorization but state should be looking for partners with experience doing this. Particularly focusing on insulin as target. This year, Dr. Pan is authoring another bill to further move things along (SB838) in partnership with the Governor, who is proposing California invest $30M to explore partnering and another $50M to establish a manufacturing plant and exploring four other drugs.
- Goal is to ID which drugs suffer the worst market failures and signal that profiteering will not be rewarded—and the state will step in.
Washington's SB5203 - Senator Karen Keiser (WA)
- States are able to network and build with each other on these types of policies—it’s part of why SB5203 was a success.
- Advocacy groups like the AARP are strong advocates for these sorts of issues.
- Built on what California did. Had been working on drug transparency and price caps (stop gap measures), but these weren’t addressing the fundamentals of the market failure. This is an antitrust issue so we have to introduce the competition to take this on.
- Bill was a bit broader than the California bill to give Washington Health Care Authority more flexibility. Wrote so that Washington can make their own or partner with California or any other state that is working similarly on this.
- Poster child is insulin, but it’s not the only drug that’s being hijacked by a group of manufactures. MS drugs are also suffering from the same issue.
Maine's SP574 - Senator Trey Stewart (ME)
- Every state is different—Maine is a small state (1.3M people) and not geographically close to these other states working on these issues.
- Was brought to Sen. Stewart's attention by a law school classmate with a son with a T1. (Connected with him over both being Republicans in law school.) He brought forward the issue as a parent of a diabetic son. This sparked the conversation about doing public medications around insulin. Attention was spotlighted on this with Martin Shkreli and other price gouging.
- Brought together a lot of stakeholders in Maine—created an informal commission. Got a bill title in last year that carried over to this year as we worked in the interim to work on the proposal.
- Rethinking how we can provide this drug to Mainers at a lower cost—worked with the research institution at University of Maine and also some of the private sector groups doing work to compete with the big producers.
- And also looked at interstate compacts. Worried Maine might not have a big enough market, so looking to collaborate across states and regions to make the numbers work for standing something up with the state's blessing.
- Rather than pull a lever that says “the state will do it all,” we are exploring options. The bill has passed and created a formal commission and have the support of the government to do further research.
- Also petitioning the federal government to look at this as well.
California Implementation - David Toppelberg (Project Manager, CalRx)
- Flagship project: biosimilar insulin. CalRx empowers the state to become a pharma producer. Originated as an executive order from Gov. Newsom and then codified into law.
- CalRx obtained project partners at public institutions (Johns Hopkins teams looked a savings for payers and payees / patent experts).
- Made a broad survey of relative stakeholders to select which drugs to target — took stakeholder considerations and combined with user data from California health networks.
- Top of the list: insulin, which had large demand, high costs, small producer list.
- State will invest $50M into biosimilar insulin and another $50M to support a manufacturing facility and keep production close to the population. Three benefits team is looking for: (1) priority access; (2) branding (California-related branding), as labeling will create brand awareness and demonstrated the state’s commitment; and (3) low cost implementation: partnerships with contract manufacturing are likely the lowest risk and lowest costs. They would be responsible for roll out and manufacturing.
- Reflections: not doing direct manufacturing — the state is not equipped to do. But not looking for a traditional procurement contract. Making a hybrid/partnership model to bringing drugs to market. [Resource recommended by Dana Brown: “Deploying the Government Owned, Contractor Operated Model”]
- Distribution is the big challenge. It’s one thing to make a drug, it’s another to get it to people.
Washington Implementation - Donna Sullivan (Chief Pharmacy Officer, WA HCA)
- Had numerous conversations with the state of California - interest in following their lead on contracting with a manufacturer: to create a public manufacturing cooperative as a possibility.
- Also looking at Utah’s solution: creating a discount card through residents there. Looking at procurement for negotiating a steep discount with current existing insulin products.
- Focusing on all Washington citizens, not just state employees or public option users. Medicaid federal rebate rules make this difficult to consider.
- Some challenges will be distributing to pharmacies and if a pharmacy would have to keep two different inventories. In researching phase now—closer to doing the discount card (net rebate) than to a partnership.
Q&A: What can smaller states do?
- Dana Brown: There are small scale productions in cities and countries around the world. Public university system in Colombia, for example, makes immunotherapy at patient's bedside. Having a state as large as California hopefully gives other states insights into how they work going forward. [See Dana's "Medicine for All" for more examples.]
Q&A: Who are the groups that can support a bill like this? And which groups opposed this?
- Sen. Keiser: Great support from T1International and diabetic advocacy, as well as retiree groups (AARP are very involved in high prescription drug costs). Medicare and federal rules can get in our way for some issues. One group that we didn’t bring in soon enough: retail pharmacies (the smaller ones). The fact is: They are the dispensers of most drugs in the country. They have great anxiety about how to stock and distribute the drugs that come from different manufacturers. (ex. We wanted to ask pharmacies to have an emergency stash of insulin and there wasn’t consensus on what brands or types to have.)
- Sen. Stewart: Didn’t have much opposition because the pharma companies realized it’s a little state that cannot do that much in a non-budget year. As things grow and expand, we’re likely to see more pushback at the committee process. We have folks (OpenInsulin and a few others) who helped us in the process. And local experts, hospital experts, research institutions.
Q&A How big could this go? Could they sell to folks outside of their state?
- Dana Brown: Publicly produced meds from one state could be sold to other states. It’s all about creativity and solidarity to find workable solutions in the short term. Lots of civic creativity potential here.
Stay tuned for our next briefing, on Restorative Justice, on Friday, May 20 at 1PM ET
The current criminal legal system fails to address the needs of harmed parties, offending parties, and communities writ large. A greater integration of and financial support for restorative justice processes throughout the criminal legal system, however, has the potential for transformative change. Taking many forms, from victim-offender dialogues to community conferences, this approach to harm rejects retribution and instead acknowledges the diverse needs of harmed parties, offending parties, and their communities alike. Fortunately, many cities and states are experimenting with new forms of restorative justice, from Colorado's Restorative Justice Coordinating Council to Vermont's Community Justice Centers. Join us to learn from experts and advocates at the frontier of advancing this model.
Speakers: Nketiah Berko (Democracy Policy Network), Sharletta Evans (Colorado Crime Survivors Network, Inc.), Thalia González (Occidental College), Jessica Persaud (Common Justice), Liz Porter-Merrill (Colorado Restorative Justice Council), Dr. Shannon Sliva (University of Denver), Sen. Pete Lee (CO)

